Common Signs of the New Flu in Adults and What to Watch For
Outline:
1) Signs Of The New Flu In Adults: the core symptom picture and how it differs from colds and other viruses
2) Early Signs Of The New Flu Virus: the first 24–48 hours and practical detection tips
3) Warning Signs Of Severe New Flu: red flags that require urgent evaluation
4) Home Care: Comfort, Recovery, and Reducing Spread
5) Prevention, Risk Factors, and Community Awareness, with a closing takeaway for adults
Signs Of The New Flu In Adults
When a new flu strain circulates, adults often ask the same question: what does it look and feel like in real life? The overall picture tends to be brisk and body-wide. Many adults report a sudden “hit by a truck” sensation within hours, not days, with fever, deep muscle aches, and head pressure announcing themselves in a sharp arc rather than a slow burn. In plain terms, the onset is typically abrupt, and the constellation of symptoms skews systemic. What the guides say about the new flu symptoms is that the core pattern remains familiar to seasonal influenza even as details shift with each strain.
Typical features in adults include the following clusters:
– Systemic: fever (often 38–40°C/100.4–104°F), chills, sweats, severe fatigue, and prominent body aches.
– Respiratory: dry cough that may become productive, sore or scratchy throat, and nasal congestion or runny nose.
– Neurologic and sensory: headache behind the eyes, light sensitivity in some cases, and a “foggy” feeling.
– Gastrointestinal: nausea or loose stools can occur, though these are less common in adults than in children.
Compared with the common cold, the new flu tends to come on faster and hits harder below the neck. Colds often begin with a mild sore throat and stuffy nose that build gradually; flu usually announces itself with fever and aches first. Distinguishing from other viruses also matters. Sudden loss of smell or taste, for example, is more strongly tied to other respiratory infections and is not the hallmark feature of flu. Adults should also note the typical timeline: incubation commonly spans 1–4 days after exposure, with the first three days of illness being the most intense for fever and aches. Transmission risk peaks early as well, often beginning about a day before symptoms and continuing for roughly a week, longer if someone is immunocompromised. While each strain brings small twists—such as cough prominence or greater sore-throat intensity—the classic adult profile of abrupt fever, fatigue, and widespread aches remains a reliable anchor for recognition.
Early Signs Of The New Flu Virus
The earliest signals can be subtle, arriving like the quiet wind before a storm. You may notice an inexplicable dip in energy during the afternoon, a wave of chills without much fever yet, or a background ache in the legs and lower back that feels “deeper” than a post-workout soreness. A scratchy throat might appear alongside mild headache and a sense that your usual coffee or tea no longer lifts the fog. Within 12–24 hours, these hints often surge: fever climbs, aches broaden, and the cough becomes more insistent.
Key early markers adults report:
– Sudden fatigue out of proportion to your day’s workload.
– Chills or sweats with a temperature beginning to edge upward.
– Diffuse muscle ache, particularly in the thighs, back, and shoulders.
– A tight, dry cough or an irritable throat that makes speaking feel effortful.
– Appetite dipping and sleep becoming unusually heavy or restless.
These early signs help differentiate flu from allergies (which favor itchy eyes and sneezing) and from many colds (which start milder and focus on the nose). Incubation is typically 1–4 days, and viral shedding is often highest around symptom onset, which is why acting early helps protect others. Hydration and rest in the first 24 hours can reduce discomfort, and a plan for reducing exposure—masking when around others, improving ventilation at home, and pausing social visits—can meaningfully cut spread while you clarify what’s unfolding.
When to seek advice is an essential piece of the early picture. Contact a clinician promptly if you are pregnant, over 65, living with chronic heart or lung disease, diabetes, kidney disease, or conditions that affect your immune system. Early evaluation can open a window for prescription antivirals, which are time-sensitive and may reduce the risk of complications. If you care for someone at higher risk, or work in settings with close contact, an early conversation with a healthcare professional can also guide testing and return-to-work decisions. Early, calm action—rather than waiting for a full-blown fever—often pays dividends in safety and comfort.
Warning Signs Of Severe New Flu
While most adult cases remain moderate and self-limited, a minority progress and require urgent attention. The danger signs reflect either respiratory compromise, dehydration, or involvement of vital organs. Trust your senses: a fever that won’t budge, breathing that feels strained, or a mental state that shifts from tired to confused are not typical “ride-it-out” features. The sooner red flags are recognized, the sooner targeted care can begin.
Seek urgent evaluation immediately if you notice:
– Shortness of breath at rest, rapid breathing, or chest pain/tightness.
– Oxygen readings that are low for you if you monitor at home, or a bluish tint to lips.
– Severe or persistent fever above 40°C/104°F despite fluid intake and rest.
– Confusion, difficulty waking, new dizziness, or fainting.
– Inability to keep fluids down, signs of dehydration (very dark urine, minimal urination, dry mouth).
– Worsening cough with high fever after initial improvement, which can signal bacterial pneumonia.
– Severe weakness, new leg swelling, or a pounding heartbeat that feels out of proportion.
Complications of severe flu can include pneumonia, exacerbation of asthma or chronic lung disease, inflammation of the heart muscle, and rarely neurologic involvement. Adults with cardiovascular disease, chronic lung disease, metabolic conditions, pregnancy, or immune suppression carry a higher baseline risk. In these contexts, even “moderate” symptoms deserve a lower threshold for in-person assessment. Timely use of prescription antivirals and supportive therapies can change the trajectory when started promptly.
Self-care basics and safety considerations still matter while arranging care: avoid driving yourself if you feel lightheaded, focus on small, frequent sips of fluids to prevent dehydration before transport, and keep a simple list of your symptoms and their timing to share on arrival. If you live alone, notify a friend or neighbor that you are unwell and keep a phone nearby. Severe flu is not a test of endurance; it is a cue for coordinated action supported by professionals.
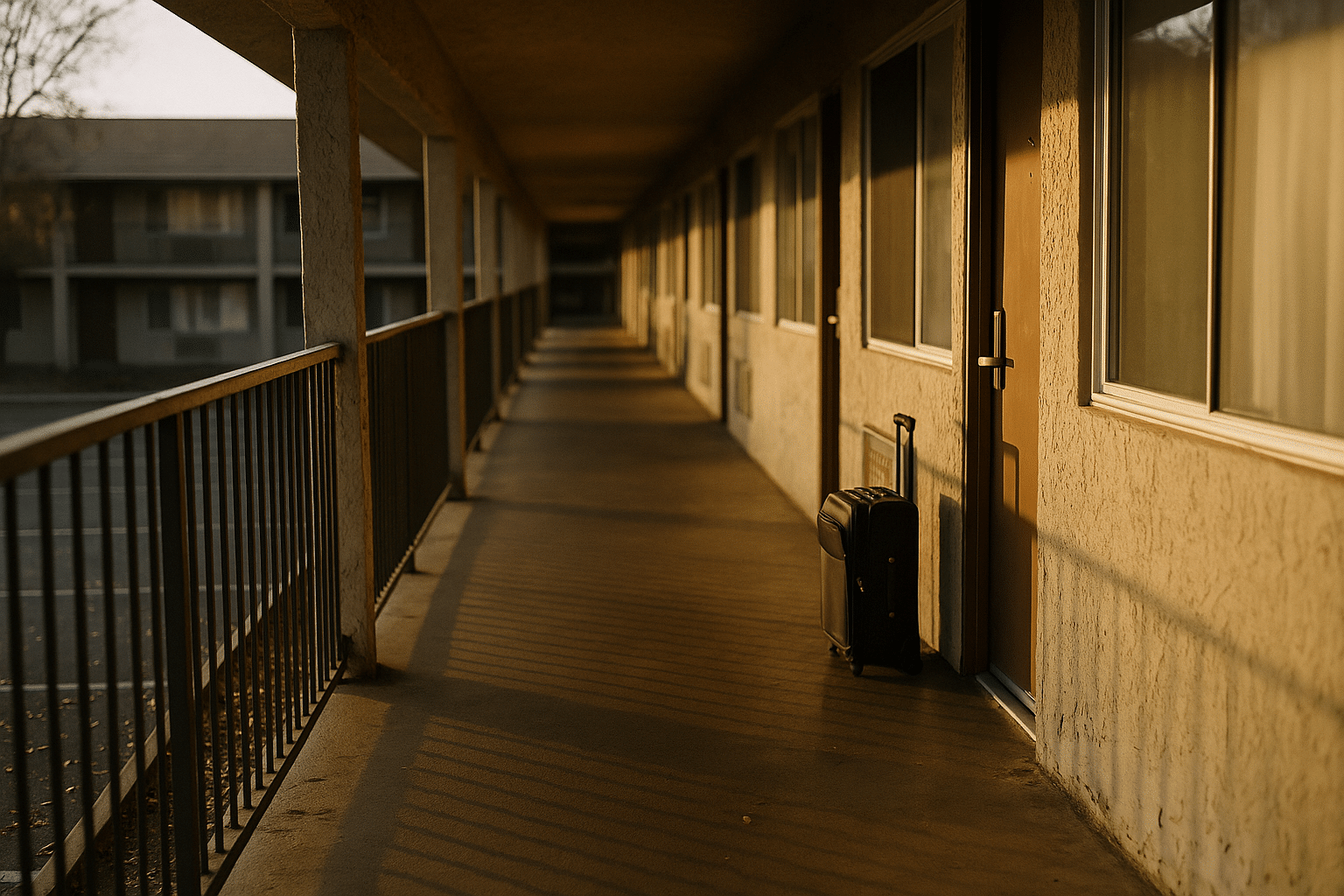
Home Care: Comfort, Recovery, and Reducing Spread
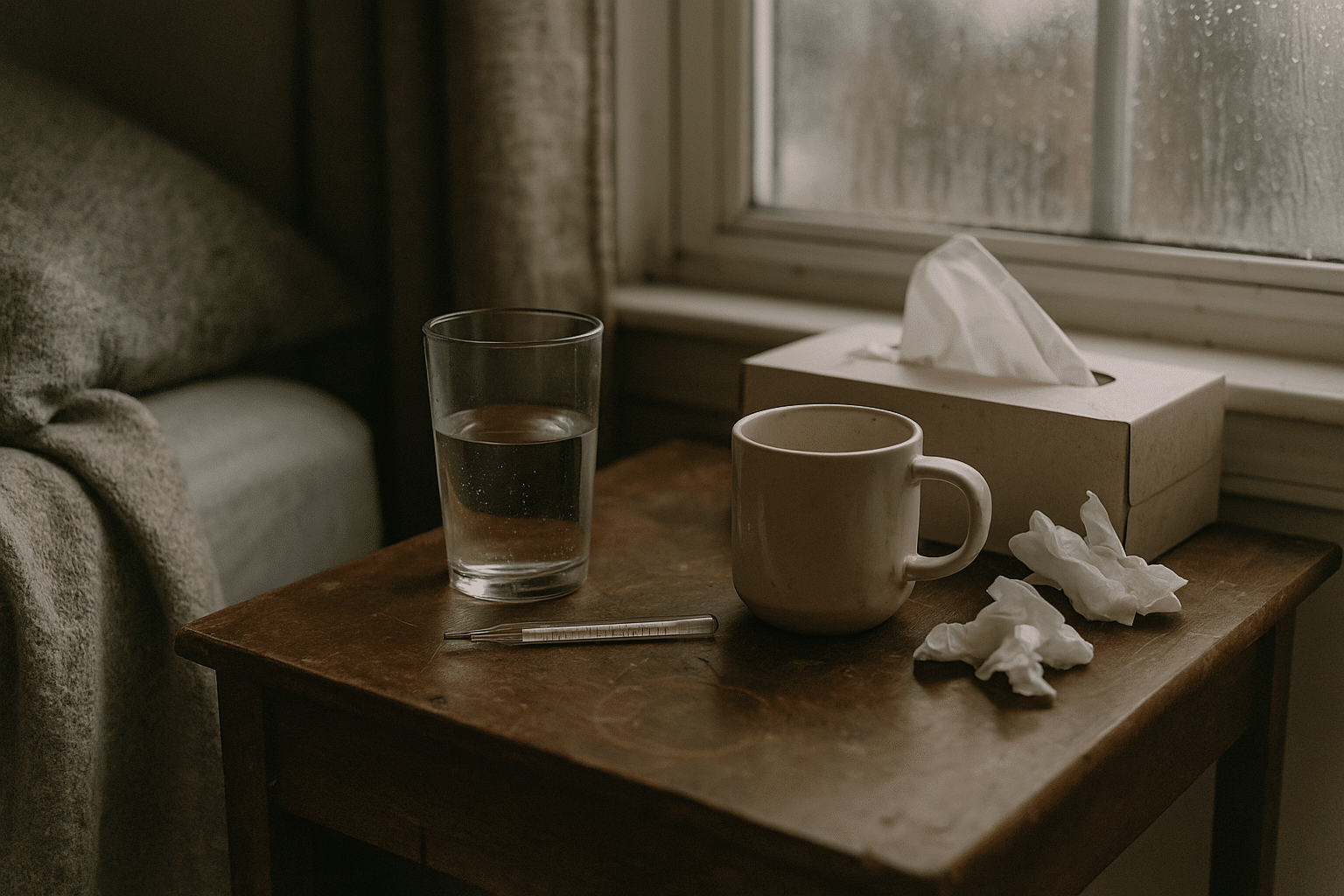
For the majority of adults, recovery at home is feasible and effective, especially when the first 72 hours are handled with intention. Practical steps for home care begin with rest that respects your body’s signal to slow down. Think of your energy like a battery that charges best when the device is idle; pushing through fevers and aches often prolongs the arc of fatigue. Create a “recovery zone” with water within reach, extra tissues, a humidifier if available, and a lined trash bin so you can minimize trips and reduce contact with shared spaces.
Evidence-informed home measures:
– Hydration: aim for steady sips; broth, water, and oral rehydration solutions help replace fluid and electrolytes. Dark urine or dizziness on standing suggests you need more.
– Fever and pain relief: use over-the-counter options as directed on the label; these can reduce discomfort but do not cure the infection.
– Cough and throat care: warm drinks, steam from a shower, and lozenges can ease irritation; a cool-mist environment may help with nighttime cough.
– Nutrition: small, simple meals—soups, bananas, rice, toast—are often easier when appetite dips.
– Sleep: short, frequent naps may be more realistic than long stretches; elevate the head to ease cough.
To limit spread at home, open windows for short bursts to refresh air, wear a well-fitted mask when leaving your room, and clean high-touch surfaces like doorknobs, remotes, and faucets. Isolate to one bedroom if possible, and use a separate bathroom or clean shared bathrooms after each use. Place a laundry bag inside your room for tissues and linens; wash hands after handling them. Most adults begin to feel better after 3–5 days, though cough and fatigue can linger beyond a week. Resume activity gradually; a simple rule is that if your symptoms worsen with activity, you’re not ready to ramp up yet. Finally, check in with a clinician if fevers persist beyond four days, if your cough deepens rather than lightens, or if any new chest symptoms emerge. Thoughtful, steady care buys comfort and reduces the chance of setbacks.
Prevention, Risk Factors, and Community Awareness
Prevention is both personal and communal—the choices you make at home ripple outward to coworkers, friends, and neighbors. Safety and prevention strategies are most effective when layered rather than treated as a single silver bullet. Vaccination against circulating influenza strains remains a cornerstone of reducing severe outcomes, particularly for older adults and those with chronic conditions. In addition, prompt testing and early treatment decisions in higher-risk individuals can narrow the window for complications. Good ventilation, hand hygiene, and staying home when sick are pragmatic tools that pair well with seasonal vaccination to curb spread.
Daily prevention habits that add up:
– Wash hands with soap and water for at least 20 seconds after coughing, sneezing, or returning home; use sanitizer when sinks aren’t available.
– Improve airflow by opening windows when weather allows or spending time outdoors when feasible.
– Cover coughs and sneezes into your elbow or a tissue; dispose and wash hands right away.
– Clean high-touch surfaces regularly, especially during household illness.
– Consider a well-fitted mask in crowded indoor spaces during peak flu circulation or when you’re recovering.
Recognize risk contexts: workplaces with close quarters, public transit during rush hours, and large indoor events all increase exposure opportunities. If you live with someone at higher risk, discuss a household plan before anyone is ill: who will pick up supplies, which room can serve as a recovery space, and how to adjust routines temporarily. Keep a modest stock of essentials—thermometer, fever reducers, electrolyte packets, tissues—so you’re not scrambling while symptomatic. For travel, check local health advisories and consider timing trips outside peak flu waves if your schedule allows. Above all, pair practical steps with awareness; small, steady habits performed consistently beat occasional heroic efforts.
Conclusion: What Adults Should Remember
Flu signals arrive fast, and recognizing the pattern is half the battle. Early action, measured self-care, and clear thresholds for professional input keep most adults on a safe track. Protect your circle with simple, repeatable prevention steps, and give your body time to mend before returning to full speed. The goal is not perfection; it is thoughtful progress from first symptom to full recovery.